Background
Although public health expenditure is low in Nigeria, healthcare purchasing has been predominantly passive and inefficient, meaning that limited resources are wasted (Etiaba et al., 2018). Recent health financing reforms in Nigeria recognize the critical roles of State governments and related agencies in defining, implementing and managing healthcare purchasing functions within decentralized health financing mechanisms; in the hope that a decentralized approach will fast-track the country’s achievements of universal health coverage (UHC) by 2030 (Chu et al., 2019). In Abia State, healthcare has been predominantly financed through out-of-pocket payments (OOP) and State government budgetary allocation. The State has recently established a health insurance agency with plans to roll-out a mandatory contributory social health insurance scheme for all citizens and residents within 2020. In this blog, we review provider payment mechanisms (PPMs) used by the state’s health budget and the proposed Abia state social health insurance scheme and provide recommendations to harmonize the multiple and mixed PPMs.
Provider payment mechanisms
- Budgetary allocation for health
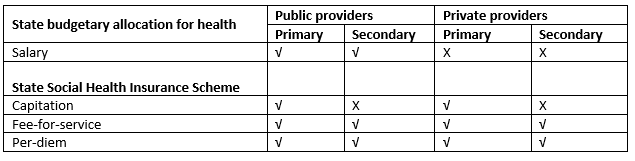
The State health budget pays salaries to health workers and staff of agencies in the public health sector, including the Ministry of Health, State Primary Healthcare Development Agency, State Health Insurance Agency, General Hospitals and Primary Health Centers. The salary is a fixed payment to the service provider every month for services rendered. Salaries vary depending on the cadre and rank of the staff, but is not linked to provider performance.
- State Social Health Insurance Scheme
Abia’s social health insurance operational guideline stipulates that public and private providers will be contracted for primary and secondary healthcare services. Primary public and private providers are entitled to capitation, fee-for-service and per diem while secondary providers are paid via fee-for-service and per diem. Capitation is advance payment of a predetermined fixed amount, for a specific package of services, for a defined duration and population registered with the provider. Fee-for-service (FFS)is a payment per service rendered for referrals and emergency cases. Per-diem is a daily payment for each day of hospitalization.
Table 1 shows the PPMS in use by level of care and provider type for the two health financing mechanisms.
Table 1: Current and proposed provider payment mechanisms
The potential influence of PPMs on provider behavior and SHP
Abia State has multiple PPMS which overlap across the levels of care (primary and secondary) and provider type (public and private). Public providers are entitled to capitation, fee-for-service under the state health insurance and also receive monthly salaries from the state budget. These PPMs are not harmonized and instead duplicate coverage and payment of services. FFS reimbursements may incentivize providers to increase the number of services delivered, above what is medically necessary, leading to supplier-induced demand and increased reimbursements from the purchaser (Ikegami, 2015). Per-diem could incentivize providers to raise the number of hospital admissions (including unnecessary admissions) and increase the length of hospital stay for in-patients since hospitals are not required to supply information about actual clinical activities (Berensen et al., 2016).
Multiple sources of funds flow provide collateral pathways for health facility funding, but evidence shows that multiple and mixed PPM produce negative provider behaviors. Providers are attracted to shift clients, services and resources from less profitable to more profitable payment mechanisms (Largarde et al., 2010; Frakt, 2011; Onwujekwe et al., 2019). Onwujekwe et al. (2019) in their study of public tertiary hospitals, found that in order to claim FFS reimbursements, in addition to the prepaid capitation, some providers were incentivized to offer unnecessary laboratory services to clients who only required primary level care (Onwujekwe et al., 2019). These negative provider behaviors result in cost escalation, resource wastage and inefficient utilization of limited resources to provide quality health services for those in need. These consequences negatively impact clients who will invariably be exposed to differential standards of care and unequal access to health services.
Recommendations
To minimize the negative influence of mixed and overlapping PPMs on provider behavior and enable progress towards SHP the following recommendations are made:
- PPMs should be harmonized and linked to outputs. For example if salaries are paid to health workers, additional payment may be linked to performance measured through client surveys.
- Where it is not possible to restrict the number of funding flows, controls should be instituted such as,
- Gate-keeping, such that first visits to primary providers are incentivized (e.g. fully covered by the scheme) and non-emergency cases, that can be managed at the primary level, presenting to secondary health facilities are disincentivized (e.g. not covered by the scheme)
- For per-diems, transparency to the public of the cost of admissions across hospitals will offer consumers the potential for cost-comparison. There should also be on-going, and retrospective reviews of medical records for hospital stays to inform decisions about denial of payment for unnecessary hospital stays
- Fee schedules should be periodically reviewed to clearly define and set fees as well as the conditions of billing. Strict audit of adherence to billing requirements should be implemented to control cost and volume, as well as better quality of care for clients.
- Strict monitoring of providers and verification of claims using electronic patient registers and claims management software. This will contribute to improved provider performance monitoring.
References
Annie Chu, Soonman Kwon & Peter Cowley. (2019). Health Financing Reforms for Moving towards Universal Health Coverage in the Western Pacific Region, Health Systems & Reform, 5:1, 32-47, DOI: 10.1080/23288604.2018.1544029
Etiaba E, Onwujekwe O, Honda A, Ibe O, Uzochukwu B, Hanson K. (2018). Strategic purchasing for universal health coverage: examining the purchaser-provider relationship within a social health insurance scheme in Nigeria. BMJ Global Health, 3(5).
Berensen, RA, Upadhyay DK, Delbanco SF, Murray S. (2016). Per diem payments to hospitals for in-patient stays (In) Payment Methods and Benefit Designs: How they work and how they work together to improve health care. Research Report. Urban Institute.
Ikegami N. (2015). Fee-for-service payment – an evil practice that must be stamped out?. International journal of health policy and management, 4(2), 57–59. https://doi.org/10.15171/ijhpm.2015.26
Onwujekwe O, Mbachu C, Ezenwaka U, Arize I, Ezumah N. (2019). Characteristics and Effects of Multiple and Mixed Funding Flows to Public Healthcare Facilities on Financing Outcomes: A Case Study From Nigeria. Frontiers in Public Health, 7:403
AUTHORS

Chinyere Ojiugo Mbachu is a community health physician in the University of Nigeria Teaching Hospital, and a senior lecturer in the University of Nigeria Nsukka. She is currently the grants officer of the Directorate for Research in the University. Ojiugo is a fellow of the West African College of Physicians and a founding member of the West African Network of Emerging Leaders in Health Policy and Systems Research (WANEL). She has published numerous articles in reputable journals, in the areas of health services, policy and financing, as well as implementation science.

Chinyere Cecilia Okeke (nee Onuh) graduated from College of Medicine, University of Calabar in 2007. She has an MPH from University of Nigeria (2015). She is a fellow of the West African College of Physicians (2016). She is also a WHO Health Policy Analysis fellow (2019). She is a lecturer with the Department of Community Medicine, College of Medicine, University of Nigeria, Enugu Campus and a researcher with the Health Policy Research Group of the same University. She has attended and presented several papers at numerous conferences and published articles in peer reviewed journals. She is happily married with children.

Irene Ifeyinwa Eze is a Consultant Public Health Physician and Lecturer at Alex Ekwueme Federal University Teaching Hospital Abakaliki, Nigeria. She is a fellow of the West African College of Physicians in Community Health. She has master’s degrees in Medical Microbiology, Public Health and Health Policy and Systems. Her research interests include Epidemiology, Maternal and Child health, and Health Policy and Systems. She is a member of various national and international professional associations including Health System Global (HSG).

Chinonso Obayi holds a master of science degree in Health Policy, Systems and Management from University of Nigeria. His research interests include health policy analysis, health financing and implementation research. His current work focuses on designing and testing community-embedded interventions for improving adolescent sexual and reproductive health in south-east Nigeria.

Professor Benjamin S.C. Uzochukwu is a Public Health Physician at the University of Nigeria Teaching Hospital Enugu and Professor of Public Health, Health Policy and Systems, University of Nigeria, Nsukka where he was the founding Director of the Institute of Public Health. He is the National President of the Association of Public Health Physicians of Nigeria (APHPN), Director of Grants and Research West African College of Physicians (WACP) and member of the Ministerial Expert Advisory Committee on COVID-19 Health Sector Response (MEACoC).

Obinna Onwujekwe is a Professor of Health Economics, Systems and Policy, and the Director of the Directorate for Research in the University of Nigeria, Nsukka. He is the founder and Director of the Health Policy Research Group, which is a renowned and reputable research organization. He has led the development of many health policies in Nigeria, including the National Health Policy (2016) and the National Health Financing Policy (2016). He has served on the scientific and advisory boards of the African and International Health Economics.