Country context:
Population ( 2019): 47,564,296
GDP per capita ( 2018): $1710.51
THE per capita ( 2016): $78.6
Public expenditure as % of THE (2016) 37.0%
Private expenditure as % of THE (2016) 39.6%
Donor spending as % of THE (2016) 23.4%
Health Insurance coverage (2018): 20%
Country SHP objectives and priorities:
1. Progressively increase the percentage of Kenyans with coverage for essential health services.
2. Progressively expand the benefit package.
3. Improve the quality of health services.
4. Enhance financial risk protection and financing for health.
Purchasing Functions:
External Factors
• Low levels of government funding continued over reliance on OOP
• Fragmented pooling arrangements
• Weaknesses in t he legal and policy framework for the health financing system
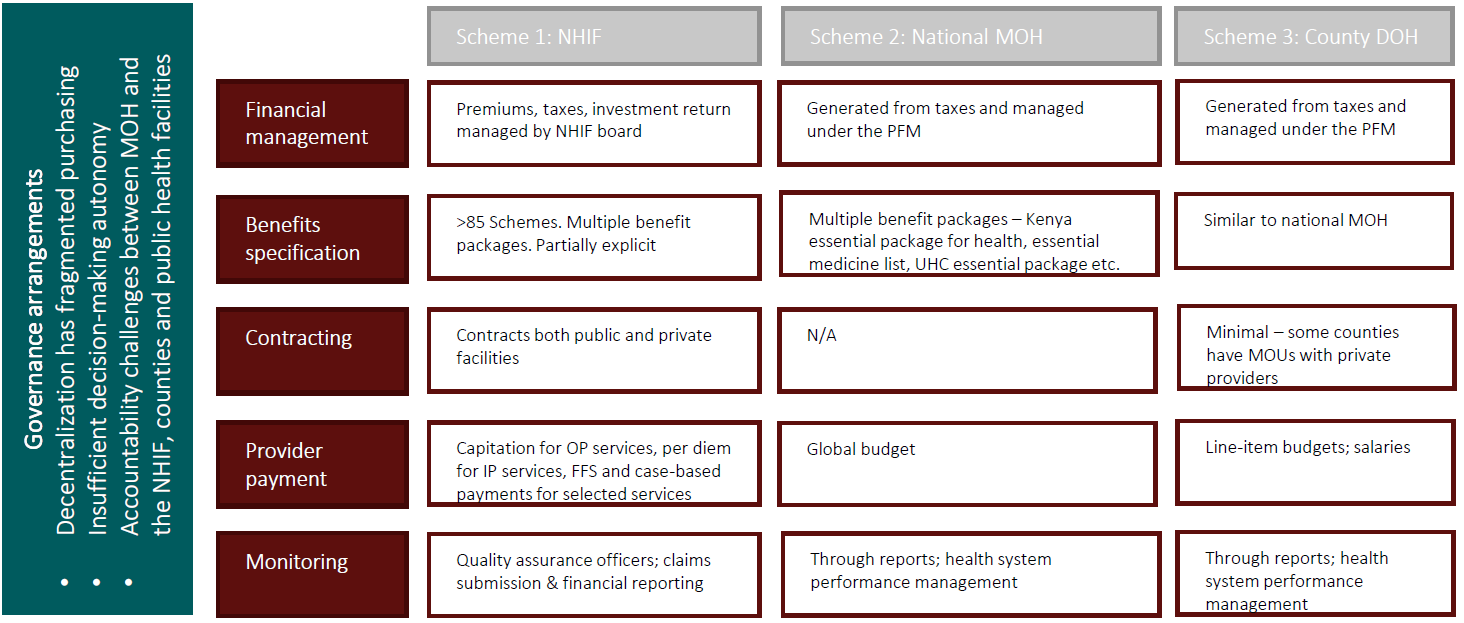
FFS Fee for service; PFM Public Finance Management; OP Outpatient; IP Inpatient
MOH Ministry of Health; DOH Department of Health; OOP Out of pocket payments
Opportunities:
Ongoing reforms (UHC & NHIF) present opportunities:
1. UHC reforms Ongoing UHC reforms are an opportunity to reform purchasing drawing on the findings of the SHP mapping.
2. NHIF reforms ongoing NHIF reforms provide an opportunity to draw on the SHP findings to strengthen NHIF purchasing.
Also, existing gaps present opportunities:
1. Information system strengthening.
2. Public financial management and effective purchasing arrangements.
3. Quality improvement: Approaches to incorporate processes and outcomes to measuring quality of care.
Next Steps
1. Dissemination of findings.
2. Cultivate local community of practice on SHP.


