Primary Health Care (PHC) is considered one of the critical components of the journey leading towards achieving Universal Health Coverage (UHC). From this perspective, the World Health Organization (WHO) encourages all countries to continue investing at least 1% of their gross domestic product for primary health care (PHC) as the surest way to make progress on universal health coverage.
In Rwanda, the agenda towards achieving UHC has registered significant progress over the last two decades and is one of the few developing countries on course to achieve UHC. Several factors contributed to Rwanda’s progress. First, Rwanda’s progress is primarily linked to the successful implementation and national scale-up of Community Based-Health Insurance(CBHI) for the informal sector. The CBHI has allowed Rwanda to have approximately 90% of its population covered by health insurance. Secondly, high coverage of health insurance boosted access to essential PHC services and is believed to have contributed to Rwanda’s achievement of the health-related Millennium Development Goals(MDGs).
Another critical factor is the bold reforms undertaken in the reorganization of the national health system to align with the national decentralization policy, which sought to achieve three main goals: promotion of good governance; poverty reduction; efficient, effective and accountable delivery of services. Drawing from these three goals of the decentralization policy, the Rwanda Health System was restructured to strengthen Referral Hospitals at the national level, create Provincial Hospitals at the Provincial level, have at least one District Hospital per District, at least one Health Center per Sector, and a Health Post in each Administrative Cell. At the Village level, a Community Health Worker Program was established to link PHC services provided by health centers with the community.
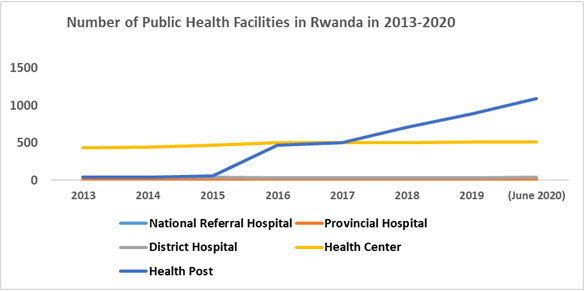
The restructuring in 2005 was motivated by the need to deepen the decentralization of and improve geographical accessibility to health services. There were only 9 Health Posts in Rwanda in 2008. The plan to expand the construction of Health Posts in Cells without any other type of Health Facility was scaled up from 2012. That decision was made based on an analysis of the access to PHC services, as presented in the Rwanda Health Sector Strategic Plan 2013–2018. The analysis concluded that while CBHI was actively reducing financial barriers to the PHC, further improvements on PHC coverage would depend on improvement to geographical accessibility, measured by reducing the average time to reach the nearest health facility. To that end, the new policy orientation adopted was to increase the number of existing levels of public health facilities, emphasizing, in particular, the scale-up of health posts[1] in administrative cells without any other level of health facility. In addition to the analysis on access to PHC services, the Integrated Household Living Conditions Survey conducted in Rwanda in 2006 indicated that it took a Rwandan citizen an average of 95 minutes to walk to the nearest Health Facility.
1. Implementation of the Rwanda Health System Restructuring
To decrease the long distance to travel to Health Facilities to access PHC, the Government resolved to construct additional Health Facilities, including new District Hospitals in Districts that did not have one and new Health Centers in Sectors that did not have any health centers. Between 2005 and 2017, 91 new health centers were built countrywide, and the number of health posts increased from 9 to 505. The construction of new health centers and health posts resulted in a substantial decrease in the average time to reach the nearest health facility. It reduced from 95.1 minutes in 2006 to 49.9 minutes in 2017. The observed contribution of the health posts in the reduction of the average time to reach the nearest health facility further convinced the Government and the Ministry of Health of the need to accelerate the construction of new health posts. Thus, from 2017 to 2020, additional 589 new health posts were built countrywide. By July 31, 2022, there were 1,160 operational health posts in Rwanda.
2. Scope and management of Health Posts
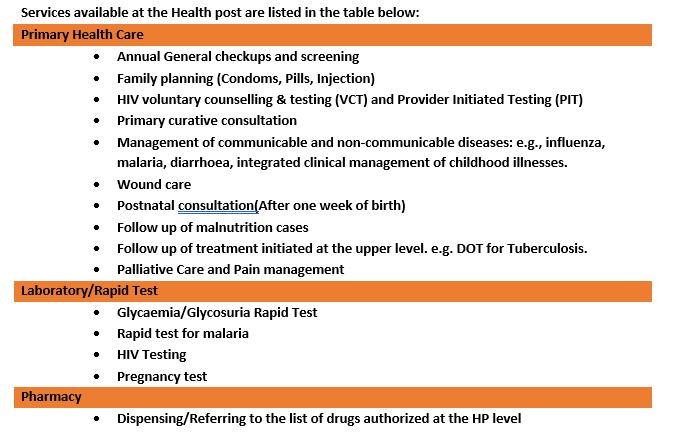
A health post is the lowest level of health facility. It provides preventive, promotional and some curative primary healthcare services. There are two models for the management of health posts. The first model includes health posts operating like the extension of a health center’s services in very remote areas. The management of these health posts is under the direct supervision of a health center within the same catchment area. The health center supervising such a health post is responsible for the facilitation and control of all operations and transactions at that health post.
The second model of management includes health posts managed under Public Private Community Partnership (PPCP) contracts. These are health posts managed by a private nurse who signs a contract with the District Local Government. The advantage of the PPCP model is that it promotes shared responsibility between the community, the local leadership, private nurses and the Ministry of Health itself. Local Government leadership and community own the premises and extensive equipment and facilitate the nurse to collaborate with the District Pharmacy and Health Insurances. The Ministry of Health has defined the service packages, standard list of equipment and drugs, and the procedure manual for operations.
Services available at the Health post are listed in the table below:
3. Contribution of Health Posts to PHC access during the COVID-19 pandemic
The immediate impact of investments made in the construction of health posts has been seen in a 47% improvement in geographic accessibility reducing the average time to reach the nearest health facility on foot from 95 minutes in 2005/2006 to 50 minutes in 2016/2017. Vaccination coverage among children aged 12 to 23 months has risen from 90% in 2010 to 96 percent in 2020, while the use of any modern contraceptive method has been increased from 45% in 2010 to 58 percent in 2020.
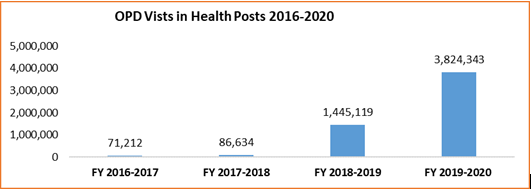
Recently, during the COVID-19 pandemic, health posts acted as the shock absorber of disruptions to services caused by the lockdown. While outpatient department consultations at health centers and hospitals declined, they increased by 260% in health posts, suggesting that services were still accessible to those seeking health services despite travel restrictions and other consequences of the pandemic.
The scale-up story for health posts in Rwanda demonstrates that PHC remains a key component of Universal Health Coverage even when the resilience of health systems is challenged. Investments like these in other African countries could make Africa’s path to UHC more realistic and sustainable.
[1] Rwanda’s Healthcare System is designed based on the country territorial administration. Rwanda is divided into four provinces plus the City of Kigali. Each province (and the City of Kigali) are further broken down into 30 districts, 416 sectors, 2148 cells and 14 837 villages. For each of these administrative entities, there is a corresponding facility responsible for healthcare delivery at its level. There are referral and specialist hospitals at the national level, provincial hospitals at the province level, district hospital at the district level, health centers at the sector level, health posts at the cell level, and community health workers at the village level.
References:
- H. Participates, “Decentralization Implementation Plan (DIP) 2011-2015,” no. January 2011, pp. 2011–2015, 2015.
- MINALOC, “Programme quinquennal de mise en œuvre de la décentralisation au Rwanda,” pp. 2004–2008, 2008.
- MINISANTE, “DOCUMENT DE POLITIQUE DE LA DECENTRALISATION DU MINISTERE DE LA SANTE,” 2003.
- Rwanda Health Sector Performance Report 2019-2020 accessed at https://www.moh.gov.rw/fileadmin/user_upload/Moh/Publications/Reports/Health_sector_performance_Report_FY_2019-2020.pdf
- Service Package for Health Facilities at Different Levels of Service Delivery -2011); Health Service Package for Public Health Facilities – January 2017; Service Packages for Upgraded Health Centers – February 2019; and the 2019 Second Generation of Health Post service package (2019)
AUTHORS

Alypio Nyandwi is a public health professional with experience in public policy analysis, planning, research, monitoring and evaluation. Alypio has over 15 years of working experience in Rwanda’s health sector, where he has worked with both governments and non-governmental organisations at the international level.

Stella Umuhoza is a lecturer and researcher at the University of Rwanda School of Public Health (UR/SPH) in the Department of Health Policy, Economics and Management. She has over ten years of experience working in public health systems. Currently, she serves as a member of the Community-Based Health Insurance (CBHI) Consultative Group and Health Financing Core Group in Rwanda. Stella recently developed Rwanda’s Health Financing Strategic Plan for 2018-2020 and the Family Planning (FP) investment case. Over the years, she has provided technical assistance to various government institutions and international organizations in developing policy documents and briefing notes to inform decision-making.

Dr Parfait Uwaliraye is the Director-General for Planning, Monitoring and Evaluation and Health Financing at the Ministry of Health in Rwanda, a position he has held since November 2012. Dr Uwaliraye is a medical doctor with a Master’s degree in Public Health. He worked as a Research Assistant, a District Medical Officer and the director of Kibagabaga District Hospital prior to joining the Ministry of Health. He has a particular focus on health policy, planning, health financing, private sector engagement and global health.

Sabine Musange F. is a lecturer and currently head of the Health Policy, Economics and Management department at the School of Public Health, University of Rwanda. With a background in both medicine and global health research, her research interests focus on strengthening health systems in low-resource settings. Previous work includes program evaluation in maternal and child health, health systems and financing. Most of her work has been carried out in low-income settings and she is passionate about women and child’s health and above all about improving population health.